VARICOSE ULCER; AYURVEDA’S GENTLE TOUCH FOR WOUNDS TO WELLNESS!
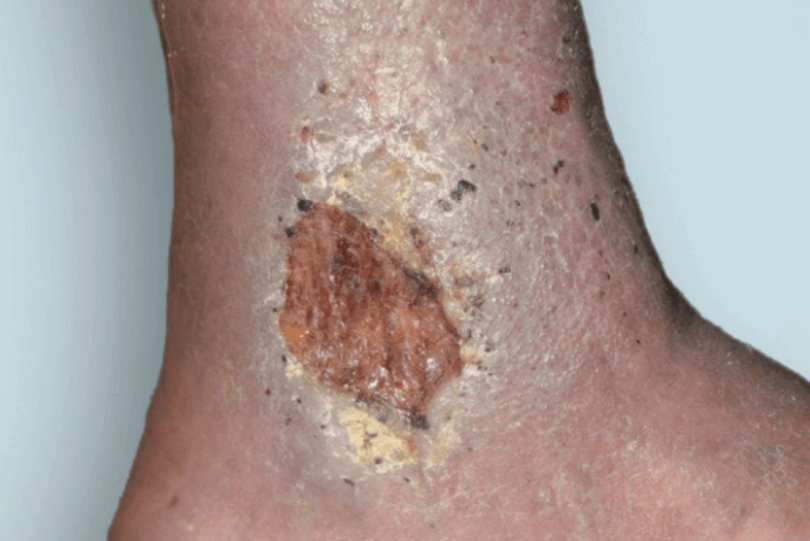
A Varicose Ulcer is a chronic, slow-healing wound that develops due to prolonged venous insufficiency(poor blood circulation in the veins). It typically occurs in the lower legs, especially around the medial malleolus(inner ankle), where venous pressure is the highest. These ulcers are often painful, have irregular borders, and may be accompanied by swelling, discoloration, and thickened skin.
In Ayurveda, Varicose ulcers are correlated with Siraja grandhi(Varicose veins) and Dushta Vrana(Chronic ulcers). Treatment focuses on improving circulation, reducing inflammation, healing the ulcer, and preventing recurrence.
CAUSES OF VARICOSE ULCER IN AYURVEDA:
According to Ayurveda, varicose ulcers arise due to an imbalance in Vata and Pitta dosha, leading to poor circulation, dryness, and tissue degeneration. Some contributing factors include:
- Excessive standing or walking.
- Chronic constipation(leading to an increased intra-abdominal pressure).
- Improper dietary habits(excessive spicy, salty, and dry food).
- Trauma or injury to the veins.
- Genetic predispositions.
CAUSES OF VARICOSE ULCERS:
There are severe complications of chronic venous insufficiency(CVI) which is commonly seen in people with varicose veins or a history of deep vein thrombosis(DVT).
1. Chronic Venous Insufficiency-CVI:
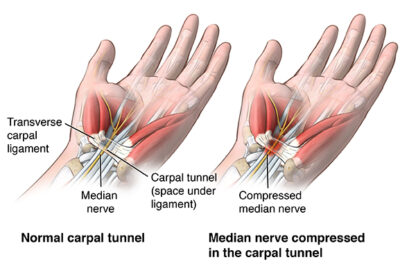
Venous ulcers occur when the veins in the lower leg fail to return blood efficiently to the heart. This leads to increased venous pressure, damaging the small blood vessels and surrounding tissues. The major causes of CVI include:
a)Faulty valves in the veins:
- Usually, veins have one-way valves that prevent blood from flowing backward.
- When these valves become weakened or damaged, blood pools in the veins, leading to increased pressure.
- This increased pressure causes damage to the skin and underlying tissue, leading to ulcer formation.
b)Varicose veins:
- Varicose veins are enlarged, twisted veins that occur when the venous valves fail to function correctly.
- The blood stagnates, increasing pressure in the veins and surrounding tissues.
- Over time, nutrient and oxygen supply to the skin decreases, making it more prone to breakdown and ulceration.
c)Deep Vein Thrombosis(DVT):
A history of DVT(blood clot in the deep veins) can damage the venous valves, leading to post-thrombotic syndrome(PTS). This condition increases the risk of venous hypertension, tissue damage, and eventually, venous ulcers.
2.Venous Hypertension(High pressure in the veins):
Increased venous pressure leads to:
- Capillary damage, causes fluid and proteins to leak into the surrounding tissue.
- Inflammation, resulting in skin thickening, discoloration, and ulcer formation.
3. Trauma or Injury:
- Even minor injuries or cuts to the skin, especially over varicose veins, heal poorly due to circulation. This can develop into a chronic ulcer, as the body cannot repair the damaged tissue efficiently.
4. Obesity:
- Excess weight increases pressure on the veins, making it harder for blood to return to the heart. This worsens venous insufficiency and can contribute to skin damage and ulcer formation.
5. Prolonged standing or sitting:
- Occupations that require long hours of standing or sitting(such as teachers, security personnel, and office workers)contribute to venous stasis, increasing the risk of ulcer formation due to poor circulation.
6. Aging:
- As a person ages, the veins and valves naturally weaken, leading to venous insufficiency and an increased risk of ulcers.
7. Smoking and alcohol consumption:
- Persistent high pressure in the venous system damages the endothelium(inner lining of blood vessels), causing inflammation and increasing the likelihood of ulcers.
8. Diabetes and poor nutrition:
- Diabetes delays wound healing and increases the risk of infection.
- A lack of essential nutrients(vitamin C, Zinc, protein)weakens skin and connective tissues, increasing ulcer risk.
8. Chronic inflammation and skin condition:
- Conditions like eczema, cellulitis, or dermatitis weaken the skin, making it prone to ulcers.
PATHOPHYSIOLOGY OF VARICOSE ULCER:
- Venous valve failure: Blood reflux and pooling in veins.
- Increased venous pressure: Fluid leaks from the vein into surrounding tissue edema.
- Chronic inflammation: Accumulation of waste products and reduced oxygen supply.
- Skin changes: Hardening, darkening(hyperpigmentation), and skin thinning.
- Ulcer formation: Even minor trauma can lead to an open wound due to poor healing.
CLINICAL SYMPTOMS OF VARICOSE ULCER:
1. Local Symptoms:
a)Ulcer characteristics:
- Location: Commonly found on the medical aspect of the lower leg, just above the ankle. Sometimes, it may appear on the lateral side.
- Shape: Usually irregular in shape.
- Edges: Sloping and not sharply defined.
- Base: Covered with yellow slough or necrotic tissue. In chronic ulcers, granulation tissue is present.
- Depth: Initially superficial but can be extended deeper if not treated.
- Discharge: Watery(serous) or purulent, sometimes foul smelling due to secondary bacterial infection.
b)Pain:
- Mild or painless in most cases, unlike arterial ulcers, which are very painful.
- If infected or deep, it may become moderately painful.
- Pain may worsen with prolonged standing and improve with leg elevation.
c)Surrounding skin changes:
- Hyperpigmentation: Due to hemosiderin deposition from red blood cells breaks down.
- Lipodermatosclerosis: Hardening of the skin due to chronic inflammation and fibrosis.
- Eczema/Stasis Dermatitis: Red scaly, itchy skin around the ulcer.
- Atrophie Blanche: White, scar-like patches on the skin, which are signs of chronic insufficiency.
d)Edema:
- Swelling of the affected leg due to venous congestion.
- It improves with elevation but worsens after prolonged standing.
e)Varicose veins:
- Visible, dilated tortuous veins around the ulcer.
- Presence of venous incompetence(valvular dysfunction) in the great or small saphenous vein.
2. Systemic Symptoms:
In most cases, systemic symptoms are mild, but in severe or infected ulcers, the following may be present:
- Low-grade fever(if secondary infection occurs).
- General malaise and fatigue due to chronic inflammation.
- Cellulitis: Infection spreads to surrounding tissues, causing redness, warmth, and swelling.
- Lymphadenopathy: Swollen lymph nodes in severe cases of infection.
3.Complications(If left untreated):
- Chronic non-healing ulcer: Can persist for months or years.
- Secondary Bacterial infection: This can lead to cellulitis or abscess formation.
- Osteomyelitis: Infection spreading to underlying bone.
- Squamous cell carcinoma(Marjolin’s Ulcer): Rare but possible in long-standing ulcers.
DIAGNOSIS OF VARICOSE ULCER:
1. Clinical Diagnosis:
A varicose ulcer is primarily diagnosed based on history and physical examination:
Symptoms:
- Chronic,non-healing ulcer on the lower leg.
- Aching or heaviness in the legs.
- Swelling in the lower legs, worse after prolonged standing.
- Brownish discoloration (hemosiderin deposition) around the ulcer.
- Itchy, scaly, or hardened skin around the ulcer(lipodermatosclerosis).
Signs:
- Shallow ulcer with irregular edges.
- Granulation tissue at the base may have a yellow fibrinous coating.
- Surrounding Skin may show pigmentation, eczema, or thickening.
- Visible varicose veins or history of deep vein thrombosis(DVT).
- Edema, which reduces elevation.
2. Diagnostic Tests:
1.Doppler Ultrasound(Venous doppler scan):
- Check for venous reflux or obstruction in deep or superficial veins.
2.Ankle-Brachial Index(ABI):
- Differentiating between arterial and venous ulcers(ABI<0.9) suggests arterial involvement.
3. Duplex Ultrasound:
- Confirms venous insufficiency and maps reflux in the venous system.
4. Wound swab or biopsy:
- In cases of suspected infection or non-healing ulcers rule out malignancy.
5. Blood tests:
- Fasting blood sugar(to rule out diabetes).
- Complete Blood count(CBC): To check for infection or anemia.
DIFFERENTIAL DIAGNOSIS:
1.Arterial Ulcer(Ischemic Ulcer):
- Cause: Peripheral arterial disease(PAD) atherosclerosis leading to ischemia.
Key Features:
- Located on toes, heels, lateral malleolus, or pressure points.
- Painful, especially at rest and at night(relieved by dangling the leg).
- Punched-out appearance with well-defined edges.
- Cold, pale foot with weak or absent peripheral pulses.
- Skin changes: Shiny, hairless skin, delayed capillary refill.
Differentiation:
- Varicose ulcers are usually on the medial malleolus with irregular borders and brown pigmentation, while arterial ulcers have a punched-out shape and are very painful.
2. Diabetic Foot Ulcer:

- Cause: Peripheral neuropathy and microvascular disease in diabetes.
Key Features:
- Usually found on pressure points like soles, metatarsal heads, or toes.
- Painless(due to neuropathy).
- Surrounded by callus(in neuropathic ulcer).
- Usual pulses unless complicated by ischemia.
- Often superinfected, leading to foul-smelling discharge.
Differentiation:
- Varicose ulcers are usually associated with venous insufficiency(swelling, hemosiderin deposits), whereas diabetic ulcers are related to neuropathy and pressure points.
3.Pressure Ulcer(Decubitus Ulcer):
- Cause: Prolonged pressure due to immobility(eg: bedridden patients).
Key features:
- Located over bony prominences(sacrum heels, ischial tuberosities).
- Deep necrotic wounds that may extend to muscle or bone(advanced stages).
- Often painless due to nerve damage.
Differentiation:
- Varicose ulcers are due to venous hypertension and commonly around the medial malleolus, while pressure ulcers are linked to prolonged pressure and immobility.
4.Pyoderma Gangrenosum:

- Cause: Autoimmune disorder(associated with inflammatory bowel disease, rheumatoid arthritis, or malignancy).
Key Features:
- Rapidly progressing ulcers with violaceous, undermined borders.
- Severe pain.
- Pustules that ulcerate quickly.
- Negative bacterial cultures(non-infectious).
Differentiation:
- Unlike varicose ulcers, pyoderma gangrenosum ulcers are painful, rapidly spreading, and not associated with venous stasis changes.
5.Marjolin’s Ulcer(Squamous Cell Carcinoma in Chronic Ulcer):

- Cause: Malignant transformation of chronic ulcers or scars.
Key Features:
- A non-healing ulcer that worsens over time.
- Indurated(hard), raised edges.
- Foul-smelling discharge.
- May have bleeding or new onset pain.
Differentiation:
- Varicose ulcers are chronic but typically respond to compression therapy, whereas Marjoin’s ulcer shows progressive worsening and induration.
6. Tuberculous Ulcer:
- Cause: Cutaneous tuberculosis(Lupus Vulgaris or scrofuloderma).
Key features:
- Slow-growing, painless ulcer.
- Undermined edges.
- Granulomatous tissue in biopsy.
- Positive Mantoux test and Chest X-ray may show Tb signs.
Differentiation:
- Unlike varicose ulcers, Tb ulcers have undermined edges, are painless, and have systemic Tb signs.
7. Traumatic Ulcer:
- Cause: Injury, burns, or repeated trauma.
Key Features:
- History of trauma.
- Variable location, depending on injury.
- No underlying vascular changes.
Differentiation:
- Varicose ulcers have underlying venous insufficiency, where traumatic ulcers are directly related to an injury.
TREATMENT OF VARICOSE ULCER IN AYURVEDA:
A)Shodhana Chikitsa:
- Detoxification is essential for chronic ulcers to remove toxins(ama) from the body and improve circulation.
1Raktamokshana(Bloodletting Therapy):
a)Jalauka Avachara(Leech Therapy):

- علاج العلقة helps to improve the blood flow, reduce swelling, and prevent clot formation. This is one of the most effective Ayurvedic treatments for venous ulcers.
b)Siravedha(Venesection):

- In some cases, venesection can be performed to remove stagnant blood and improve circulation.
2.Virechana(Purgation Therapy):
- Purgation with Triphala Churna, Avipathi Churna, or Gandharvahastha Eranda Taila is beneficial for detoxifying the body and balancing the Pitta Dosha.
B)Shamana Chikitsa(Palliative Treatment):
Internal Medications Given are:
- Patoladi Kashayam.
- Manjishtadi Kashayam.
- Sarivadyasava.
- Panchatikta Guggulu Ghrtham.
- Guggulutiktam Ghrita.
- Triphala Guggulu.
- Ashwagandha Churna.
- Kaishora Guggulu.
- Arogyavardhini Vati.
- Eranda Taila.
- Kalyanaka Ghrita.
C)Sthanika Chikitsa:
a)Vrana Shodhana:
- Cleansing the ulcer wounds with herbal decoctions to remove slough and bacteria.
- Triphala Kashaya: Effective in reducing infection and promoting granulation.
- Panchavalkala Kashaya: Bark decoction of Vata, Udummbara, Ashwatha, Parishaplaksha).
- Neem(Nimba)Decoction: Acts as an antibacterial.
b)Vrana Ropana(Wound Healing):
After cleansing, wound healing can be promoted with herbal application:
- Jatyadi Taila: Excellent for chronic ulcers.
- Dashanga Lepa: A herbal paste used for wound healing.
- Madhu(honey) and Ghee: Used as a dressing to speed up healing.
- Yashtimadhu(Licorice)paste: Soothes inflammation and aids in healing.
Diet and Lifestyle Recommendations:
1.Ahara(Diet):
- Consume blood-purifying foods like beetroot, pomegranate, garlic, turmeric, and leafy greens.
- Avoid spicy, oily, and processed food that aggravate pitta.
- Drink warm water infused with Triphala to aid digestion and detoxification.
2.Vihara(Lifestyle):
- Avoid long hours of standing or sitting with your legs down.
- Elevate the legs while sleeping to improve venous return.
- Practice gentle Yoga poses like Viparitha Karani(Legs up the wall pose) and Pavanamuktasana to improve circulation.
- Wear compression stockings to prevent venous pooling.
DISCLAIMER: The information provided in this article is intended solely for educational purposes. Treatment decisions should be made exclusively by a well-qualified Ayurvedic physician. Self-medication is strongly discouraged.
Maurya Ayurveda Hospital,opposite to Sabine Hospital,Pezhakkapilly P.O,Muvattupuzha,Ernakulam;PIN:686673,Contact no:9947183000
Email: info@mauryaayurveda.com
مركز ماوريا أيورفيدا لتقويم العظام وإعادة التأهيل العصبي (مستشفى الأيورفيدا)