ASTHMA CARE REDEFINED; BREATHE FREELY WITH AYURVEDA

Asthma is a chronic inflammatory disorder of the airways characterized by episodic and reversible airflow obstruction. It results from hyperresponsiveness of the bronchial tubes to various stimuli, leading to recurring symptoms such as wheezing, shortness of breath, chest tightness, and coughing. These symptoms are often more pronounced at night or early in the morning and can vary in intensity. It is common in children and adults and is most prevalent in urban areas.
Asthma is classified as a heterogeneous disease with multiple phenotypes( eg: allergic, non-allergic, exercise-induced) and endotypes(mechanisms underlying the condition). It affects individuals differently and often requires tailored management strategies.
PATHOGENESIS OF ASTHMA:
a)Immune system dysregulation:
- One factor contributing to inflammation is an imbalance between Th1 and Th2 lymphocytes.
- Eosinophil recruitment and excessive IgE production worsen airway reactivity.
b)Structural changes in the airway:
- Chronic inflammation causes airway remodeling, which includes enlarged muscle glands, smooth muscle hypertrophy, and epithelial damage.
c)Trigger sensitivity:
- Stress, allergen exposure, illnesses, and pollution can all cause exacerbations.
According to Ayurveda Bronchial Asthma can be correlated to Tamaka Shwasa(a type of respiratory disorder) characterized by dyspnea, respiratory distress, and wheezing.
NIDANA(CAUSATIVE FACTORS):
- Ahara(Dietary): Consumption of cold, heavy, oil, or incompatible foods.
- Vihara(Lifestyle): Exposure to dust, smoke, cold or allergens.
- Manasika(mental): Stress, anxiety, and fear.
Dosha Imbalance:
- Vata: Aggravates Prana Vayu, causing spasms and obstruction in the respiratory channels.
- Kapha: Excess mucus accumulation leads to airway blockage.
3. Other factors:
- Genetic predisposition.
- Seasonal variations(cold and damp climates).
PATHOGENESIS(SAMPRAPTHI):
- The kapha dosha accumulates and obstructs airways, impairing the normal functioning of Pranavaha Srotas(respiratory channels).
- Vata dosha gets aggravated, leading to spasmodic contractions of the bronchi and difficulty in breathing.
- It results in symptoms like wheezing, breathlessness, and cough, especially at night or early morning.
Types of Tamaka Swasa:
- Pratamaka Swasa: A severe form, often equated with acute asthma attacks.
- Santamaka Swasa: A milder and chronic condition.
CLINICAL SYMPTOMS OF ASTHMA
Airway inflammation, bronchoconstriction, and mucus production are the causes of asthma symptoms. These symptoms can be induced by physiological, occupational, or environmental causes, and they are frequently episodic and vary in intensity.
1. Wheezing:
- A high-pitched whistling sound is produced during breathing, especially when exhaling.
- It is caused by muscle tightness and inflammation that narrows the airways.
- It can be mild, moderate, or severe; in the latter, wheezing may not occur because of inadequate airflow (a medical emergency).
2.Shortness of Breath(Dyspnea):
- An inability to breathe deeply or a sensation of being out of breath.
- It usually happens at night, when engaging in strenuous activity, or when exposed to triggers.
- Having severe dyspnoea might make it difficult to carry out regular tasks.
3. Coughing:
- Coughing that is persistent or occasional, usually worse at night or in the morning.
- It may be dry or associated with the mucus (phlegm).
- Common in asthma brought on by respiratory illnesses, cold air, or physical activity.
4. Chest tightness:
- Chest feeling constricted, heavy, or under pressure.
- Frequently feeling a band-like sensation surrounding the chest.
- Caused by constricted airways and heightened respiratory effort.
5. Nocturnal Symptoms:
- Symptoms that get worse during the night, such as coughing, wheezing, or shortness of breath.
- Because of the biological clock, allergies, or flat posture, symptoms at night are frequently associated with a reduction in lung function.
6. Exercise-induced:
- Here bronchoconstriction occurs due to exertion, resulting in coughing, wheezing, or shortness of breath.
7. Episodic nature of symptoms:
- Asthma symptoms often occur in episodes, interspersed with asymptomatic periods.
- Episodes are frequently associated with exposure to triggers such as allergens, respiratory infections, or irritants.
8.Increased work of Breathing(in severe cases):
- Use of accessory muscles. (eg: neck and shoulder muscles).
- Nasal flaring, particularly in children.
- Retraction of intercostal spaces during inhalation.
- Severe airway obstruction leads to difficulty maintaining adequate ventilation.
9. Fatigue or exhaustion:
- It happens due to prolonged effort, particularly during severe or poorly controlled asthma.
- It can significantly affect daily functioning and quality of life.
ASTHMA TRIGGERS:
Asthma symptoms can triggered by:
1. Allergens:
Allergens that cause immune system overreaction, leading to airway inflammation. Common allergens include:
- Dust mites, pollen, mold(spores), animal dander, etc.
2. Environmental irritants:
Non-allergic irritants can inflame the airways or cause bronchoconstriction, worsening asthma symptoms. Examples include:
- Air pollution, smoke, strong odors or fumes, cold air.
3. Respiratory infections:
Viral or bacterial infections can exacerbate asthma symptoms by inflaming the airways. Common infections include:
- Cold and flu, sinus infections.
4. Physical Activity (Exercises induced Asthma):
- Intense exercise, especially in cold, dry air, can lead to bronchoconstriction, known as exercise-induced bronchoconstriction(EIB).
5. Weather changes:
Rapid changes in weather or barometric pressure can trigger asthma symptoms.
Specific examples include:
- Sudden cold or hot weather.
- High humidity or dryness.
6. Medications:
Certain medications can worsen asthma symptoms.
- Beta-blockers: Used for hypertension or heart problems.
- Aspirin and NSAIDs: These can trigger aspirin-exacerbated respiratory disease(AERD) in some asthmatics.
7. Emotional stress:
- Strong emotions such as anxiety, stress, or laughter can provoke asthma symptoms due to hyperventilation or airway sensitivity.
8. Food-related triggers:
- Food allergies: Peanuts, shellfish, or other allergens can induce Asthma in allergic individuals.
- Food additives: Sulfites in wine, dried fruits, or processed foods may trigger symptoms.
9. Hormonal changes:
- Hormonal functions during pregnancy, menstruation, or menopause can exacerbate asthma symptoms in some women.
10. Occupational triggers:
Exposure to specific substances at work, such as:
- Dust from wood, flour, or grain.
- Chemicals like adhesiveness, paints, or cleaning products.
- Fumes from welding or construction materials.
11. Gastroesophageal Reflux Disease(GERD):
- Acid reflux can worsen asthma symptoms by irritating the airways when stomach acid travels to the esophagus.
CLASSIFICATION OF ASTHMA:
1. Allergic Asthma(Extrinsic Asthma):
- It is the most common type and is triggered by allergens. It normally begins in childhood and is associated with other allergic conditions like eczema or fever. Normal triggers are pollen, dust mites, pet dander, molds, etc.
2. Non-Allergic Asthma(Intrinsic Asthma):
- This type is not related to allergens and often develops later in life. It is triggered by non-allergic factors such as stress, infections(e.g.: cold, flu), exercise, cold air, and air pollutants.
3. Exercise-induced Asthma(EIA) Or Exercise-Induced Bronchoconstriction(EIB):
- This type occurs during or after physical activity, especially in cold or dry conditions. The triggers are vigorous exercises, and breathing in cold, dry air during exercise.
4. Occupational Asthma:
- This is caused by exposure to irritants or allergens at the workplace.
- Its triggers are fumes, gases, or chemicals(e.g.: cleaning agents, paint), dust from flour or wood, animal fur, etc.
5. Nocturnal Asthma:
- This type worsens during the night, disrupting sleep and quality of life. The triggers related are allergens in bed(like dust and mites), cold air at night, and lying down can also aggravate obstruction.
6. Aspirin-induced Asthma:
- This is a severe reaction triggered by aspirin or nonsteroidal anti-inflammatory drugs(NSAIDs). It often occurs with polyps and chronic sinusitis.
7. Severe Asthma:
- A more severe type of Asthma that does not respond well to standard treatments like inhalers or corticosteroids.
- It involves multiple triggers like allergic and non-allergic. Often associated with other comorbid conditions(e.g.: obesity, GERD).
8. Cough variant Asthma:
- This form is characterized primarily by chronic coughing without other classic asthma symptoms. In this case, the triggers are exercise, cold air, infections, etc.
DIAGNOSIS OF ASTHMA:
Diagnosis of Asthma involves a combination of clinical evaluation, pulmonary function tests, and additional investigations to confirm the condition. Below are the primary diagnostic approaches.
1. Medical History and Physical Examination:
- Symptoms: Recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night or early morning.
- Triggers: Identification of factors that exacerbate symptoms(allergens, infections, weather changes).
- Family history: Presence of asthma allergies, or atopic conditions in close relatives.
- Exposure History: Environmental or occupational exposure to irritants or allergens is evaluated.
- Frequency and duration: Assess how often symptoms occur and if they are seasonal or persistent.
- Past medical History: Previous respiratory infections, allergic reactions, or use of medications like bronchodilators.
2. Physical Examination:
- Auscultation of the chest for wheezing.
- Signs of respiratory distress, such as rapid breathing, chest retractions, or cyanosis(bluish discoloration of skin in severe cases).
3. Diagnostic Tests
a)Pulmonary Function Tests(PFTs):
I)Spirometry:
Spirometry is a key diagnostic test for asthma.
- Forced Expiratory Volume in 1 second(FEV1): The volume of air exhaled in the first second of a forceful breath.
- Forced Vital Capacity(FVC): The total volume of air exhaled during a forced breath.
- Reversibility test: A bronchodilator is administered, and the test is repeated.Significant improvement in FEV1(>12% and >200 ml) suggests asthma.
II)Peak Expiratory Flow(PEF) monitoring:
- A simple test to measure the maximum speed of expiration using a peak flow meter.
- Variability in PEF readings(>20% difference)over time, especially after bronchodilator use or at different times of the day, supports the diagnosis of asthma.
b)Bronchial provocation Tests:
- The test assesses airway hyperresponsiveness by exposing the patient to specific triggers.
- Methacholine challenge: Methacholine is inhaled to see if it causes airway narrowing.
- Exercise-induced test: Monitoring symptoms and lung function after exercise.
c)Allergy testing:
- Skin prick or blood tests(eg: specific Ig E) to identify allergens causing symptoms.
d)FeNO Test(Fractional Exhaled Nitric Oxide):
- Measures the level of nitric oxide in the breath, which increases with airway inflammation in asthma.
e)Imaging:
- Chest X-ray: Rules out other conditions like pneumonia or structural abnormalities.
- CT Scan: Occasionally used for differential diagnosis.
4. Differential Diagnosis:
Asthma symptoms can mimic other conditions, so it’s important to rule out:
- Chronic Obstructive Pulmonary Disease(COPD).
- Vocal Cord dysfunction.
- Gastroesophageal reflux disease(GERD).
- Respiratory infections like pneumonia, and bronchitis.
DIAGNOSIS IN CHILDREN:
Diagnosing asthma in young children is challenging as they cannot reliably perform lung function tests. Diagnosis relies more on symptom patterns, triggers, and responses to bronchodilator therapy.
TREATMENT OF ASTHMA IN MAURYA AYURVEDA HOSPITAL
Our specialized Asthma treatment blends Ayurveda, physiotherapy, and acupuncture under one roof.
AYURVEDA TREATMENT FOR ASTHMA:
INTERNAL MEDICATIONS GIVEN FOR ASTHMA ARE:
- Dashamoola Kadutrayam Kashayam.
- Nayopayam Kashayam.
- Amruthotharam Kashayam.
- Balajeerakadi Kashayam.
- Amrthotharam Kashayam.
- Vasa Ghrita.
- Rasna Dashamoola Ghrita.
- Guggulu Tiktaka ghrita.
- Amruthaprasham.
- Kooshmanda Rasayanam.
- Dashamoola Rasayanam.
- Dashamoola Haritaki Lehyam.
- Matalarasayanm.
- Pippali Rasayana.
- Thamboola rasayanam.
- Vilwadi Gutika.
- Swasanandam Gutika.
- Kasturyadi Gutika.
- Chyavanaprasham.
EXTERNAL TREATMENTS GIVEN FOR ASTHMA ARE:
THALAM:

Thalam is a traditional ayurvedic treatment that involves the application of medicated paste or oil on the crown of the head. This is used when chronic or episodic asthma with stress or anxiety is a major trigger. Normally Rasnadi Thalam or Kachooradi Thalam is preferred for the same.
Benefits of Thalam for Asthma:
- It reduces inflammation.
- It aids in balancing Vata and kapha dosha.
- It improves oxygen supply.
- It reduces stress.
- Enhancement of lung function.
- It boosts the quality of sleep.
- It strengthens the immune response.
NASYAM:

Since the nose is considered as the entrance to the head, Nasyam is a panchakarma treatment that includes administering herbal oils or powders through the nostrils.
Medicated oils are used for a light massage of the head, face, and neck. The nasal pores are then opened by applying gentle steaming (Swedana) to the face and neck. The patient is requested to lie on their back with their head tilted. Next, each nostril receives a drop of the medicinal oil or powder. For the medication to take effect, the patient must relax for a few minutes. Any mucus or phlegm that gets in the patient’s throat is encouraged to spit out.
Here, we often practice two forms of Nasyam: Marsha Nasyam and Pratimarsha Nasyam.A gentler, daily-use form of Nasya therapy is Prathi Marsha Nasya. For preventative care, health maintenance, and dosha balancing, tiny doses (1-2 drops) of medicinal oil are administered. For the same reason, Anu Taila is typically preferred.
b) Marsha Nasya: This involves administering a greater volume (6–10 drops) of medicinal oil or powder via the nose. Here, we typically employ Ksheerabala Taila.
Benefits of Nasyam in Asthma:
- It clears respiratory passages.
- It reduces inflammation and strengthens airways.
- It balances Kapha and Vata dosha.
- It improves lung function and prana flow.
- It reduces allergic triggers.
- It promotes mental calmness and reduces stress.
NADI SWEDAM:

Nadi Swedam is a specialized ayurvedic sudation(sweating therapy)that uses steam generated from medicated herbal decoctions to provide heat to specific parts of the body. Here the steam can be given over the face and chest area. Halin capsule(cut open and medicine poured into water), tulsi leaves, Karpoora Thulsi Patra(leaves), and camphor are added to the water to produce steam.
Benefits of Nadi Swedam:
- It clears respiratory channels.
- It improves lung function.
- It reduces inflammation.
- It relieves muscle stiffness.
- It improves kapha imbalance.
- It enhances detoxification.
VAMANA:

Vamana(Emesis) is one of the five purification procedures(panchakarma)in Ayurveda, specifically aimed at expelling excessive kapha dosha from the body. It is a controlled process of induced vomiting to remove accumulated toxins from the upper gastrointestinal tract and respiratory system. It is performed for patients who have bala(strength).
The procedure of Vaman karma:
It is done in three stages:
- Purva karma(Pre-treatment): Preparation phase.
- Pradhana karma(main procedure): Induction of emesis.
- Pashchath karma(post-treatment): Post-procedure care.
I)Purva karma(pre-treatment):
The preparation phase ensures the body is ready for detoxification. This includes:
a)Deepana and Pachana(Enhancing digestion and metabolism):
- For 3-5 days, the patient is given digestive and carminative herbs(eg: Trikatu, Chitraka, Panchakola Churna)to improve digestion and metabolism.
- This ensures that ama(toxins)are properly digested before elimination.
b)Snehapana(Internal oleation):
- The patient is administered medicated ghee or oil(sneha Dravyas), such as Vasa Ghrita, Dadimadi Ghrita, Rasna Dashamoola Ghrita, Indukantham Ghritha, etc are given based on the patient’s condition. Normally it’s administered in about 3-7 days.
c)Abhyanga and Swedana(External Oleation and Sudation):
- Abhyanga( oil massage): Medicated oil like Karpooradi Thailam is applied over the chest region to do the massage.
- It is followed by Swedana(steaming) following the massage to open the body channels(Srotas) and mobilize toxins.
d)Specific diet(samsarjana krama):
- Before the Vamana day, the patient consumes a Kapha-increasing diet to stimulate the need for elimination.
- Like milk, yogurt, rice, jaggery, ghee, sesame seeds, heavy foods, etc.
- It aids in the expulsion of kapha during the vamana process.
II)Pradhana Karma(Main Vaman procedure-Induced vomiting):
a)Selection of time:
- The best time to perform is early morning when kapha(phlegm) is naturally dominant.
b)Administration of Vamana Dravyas:
- The patient is given a Kapha-provoking liquid such as milk or Yashtimadhu Phanta(Licorice decoction).
- Then, the main Vamana Dravyas(herbs that induce vomiting) are administered.
-Madanaphala(Randia dumetorum) churrna.
-Yashtimadhu churna(powder form).
-Vacha Churna.
-Saindhava lavana(rock salt).
-Pippali(long pepper).
c)Stimulation of Vomiting:
- After drinking the herbal liquid, the patient is encouraged to drink large quantities of warm water or decoctions.
- If necessary tickling the throat with fingers helps initiate vomiting.
- The patient expels mucus, bile, undigested food, and toxins through vomiting.
d)Observation of Samyak lakshana(Proper emesis signs):
A proper Vamana has the following features:
- Clear expulsion of kapha(thick mucus, white or frothy material).
- Lightness in the chest, clarity of senses.
- Relief from congestion, nausea, and heaviness.
III)Pashchat karma(Post-treatment and recovery phase):
a)Rest and monitoring:
- The patients are given herbal smoking therapy(Dhumapana) to prevent kapha reaccumulation.
- For this normally Haridradi varthi(turmeric wick coated with ghee)is used for the same.
b)Samsarjana krama(Diet regimen):
- A light diet is introduced gradually to strengthen digestion. Like thin rice gruel, soups, etc.
- Patients are advised a kapha-allevating diet and lifestyle to prevent recurrence.
VIRECHANAM:
Virechanam also comes under five main purification procedures(panchakarma)in Ayurveda. It is a controlled purgation therapy that eliminates toxins and doshas(mainly pitta) from the body through the intestines.
Similar to Vamana, Virechana also has three major steps:
I)Poorva karma(preparatory phase):
a)Deepana and pachana.
b)Snehapana(internal oleation).
d)Abhyanga and swedana(external oleation and sudation).
All these are done similarly to Vamana.
II)Pradhana karma(main procedure-Induced purgation):
This is a core phase of Virechana, where purgation is induced using herbal medicines.
a)Selection of Virechana dravya(Purgative medicines):
Based on an individual’s constitution(Prakrthi), disease condition, and strength, different purgative formulations are selected such as;
- Eranda taila(castor oil).
- Trivrit Lehyam(purging cassia paste).
- Aragwadhadi kashayam.
- Avipathi Choornam.
- Triphala Choornam.
- Gandharva Haritaki.
b)Administration of medicine:
- The patient is given the purgative medicine early in the morning on an empty stomach with warm water, honey, or milk.
- The dosage is determined based on the strength of the patient and the severity of the condition.
c)Monitoring the response:
- After consuming the purgative medicine, the patient starts experiencing multiple bowel movements(usually 10-15 times).
- During this time, the physician has to check for,
-The color, consistency, and quantity of stools.
-Symptoms such as burning sensation, excessive thirst, or weakness.
3.Paschat karma(Post-procedure care and diet management):
After the purgation process, the body is weak and sensitive. A proper recovery plan is essential.
a)Samsarjana krama(Gradua diet progression):
- Begin with light liquid food like kanji(thin rice porridge). Then gradually upgrade to semi-solids(thick rice porridge), soft cooked foods like lentils or vegetable soup, and finally transition to a normal diet, with easily digestible food.
- Also avoid spicy, fried, and heavy foods that can disturb digestion.
- Take rest and avoid physical exertion.
Benefits of Vamana and Virechana:
- Clears respiratory tract by expelling excessive mucus.
- Reduces frequency and intensity of asthma attacks.
- Reduces airway inflammation.
- Enhances lung capacity and oxygenation.
- Improves metabolism, reducing ama(toxins) accumulation.
- Balances Vata, Pitta, and Kapha.
- Prevents allergic asthma.
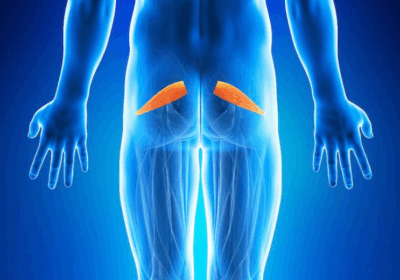
KIZHI:

Kizhi ( ‘bolus’ or ‘pouch’) contains medicinal herbal powders or other therapeutic substances. It is also a kind of Swedana(sudation therapy). For Asthma patients generally, we prefer to do Uppu Kizhi(Salt Kizhi) and Manal Kizhi(Sand Kizhi).
a)Uppu kizhi(Lavana pinda sweda):
It is a specialized ayurvedic therapy that involves the application of heated salt boluses to the body.
Asthma is primarily caused by vitiated Kapha and Vata doshas, leading to bronchial congestion, wheezing, and difficulty breathing. Benefits of Uppu Kizhi are:
- Loosens mucus(kapha Shodhana).
- Reduces inflammation(sroto hara).
- Improves lung function(Prana Vaha Srotas dushti).
- Relieves chest congestion.
- Balances Vata and Kapha.
b)Manal kizhi(Sand bolus therapy):
Manal Kizhi(sand bolus therapy) is a specialized form of Swedana(sudation therapy in Ayurveda), where heated sand is used in a cloth pouch(Kizhi) to provide therapeutic heat to the body. It is particularly beneficial for conditions where excess kapha and vata doshas cause congestion, stiffness, and impaired circulation. To prepare the Manal Kizhi, we also add Rock salt(Indupp) along with sand.
In asthma, Manal Kizhi helps in:
- Clearing mucus accumulation in the lungs.
- Reducing bronchial inflammation and improving airflow.
- Enhancing circulation, which supports better lung function.
- Pacifies Kapha and Vata doshas, the primary doshas involved in asthma.
ROLE OF PHYSIOTHERAPY IN ASTHMA:
Physiotherapy plays a significant role in managing asthma, complementing medical treatments to improve respiratory health, physical fitness, and overall quality of life. Below is a detailed explanation of the techniques and their benefits in asthma management.
1. Breathing techniques:
a)Diaphragmatic breathing:

Technique: Focuses on deep breathing using the diaphragm instead of shallow breathing using chest muscles.
- Place one hand on the chest and the other on the abdomen.
- Breathe deeply through the nose, allowing the abdomen to rise while keeping the chest still.
- Exhale slowly through pursed lips.
Benefits:
- It increases oxygen intake.
- It reduces the workload on accessory breathing muscles.
- It promotes relaxation and reduces breathlessness.
b)Pursed-Lip breathing:
Techniques: Slows down the breathing rate and helps keep airways open.
- Inhale deeply through the nose.
- Exhale slowly through pursed lips(as if blowing out a candle), take twice as long as the inhalation.
Benefits:
- It prevents airway collapse.
- It reduces shortness of breath.
- It helps maintain steady oxygen levels during an asthma attack.
c)Active Cycle of Breathing Techniques(ACBT):
Techniques: Combines breathing exercises and forced expiration to mobilize and clear mucus.
Components:
- Breathing control: Relaxed, gentle breaths.
- Thoracic expansion: Deep breaths with or without a 3-second hold.
- Forced expiration: Huffing to clear secretions.
Benefits:
- It clears mucus from the airways.
- It improves lung ventilation.
- It reduces the risk of infections.
2. Airway clearance techniques:
a)Postural drainage:
- Techniques: Uses gravity to drain mucus from specific lung segments.
- Place the body in positions where the head is lower than the chest.
- Hold the position for 5-10 minutes while breathing deeply.
Benefits:
- It promotes muscle clearance.
- It enhances airway function.
b)Percussion and vibration:
- Techniques: Manually or mechanically applied rhythmic clapping or vibrations over the chest to loosen mucus.
- Applied on the back or chest in conjunction with postural drainage.
Benefits:
- It loosens mucus for easier expulsion.
- It improves airway clearance.
3. Physical Exercise:
a)Aerobic exercises:
- E.g.: Walking, cycling, swimming, or dancing.
Benefits:
- It improves cardiovascular and respiratory endurance.
- Reduces exercise-induced asthma by strengthening the lungs.
b)Strength training:
- E.g.: Resistance exercises target major muscle groups.
Benefits:
- It enhances overall physical fitness.
- It builds strength in accessory muscles of respiration.
c)Stretching exercises:
- Gentle poses and stretches combined with breathing techniques.
Benefits:
- It improves flexibility and posture.
- It promotes relaxation and reduces stress.
4. Postural Corrections:
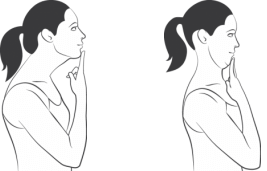
Techniques: Includes exercises to maintain and restore an upright posture.
Examples:
- Chin tucks.
- Shoulder retraction exercises.
- Stretching of tight chest muscles and strengthening back muscles.
Benefits:
- It optimizes lung expansion.
- It prevents chest tightness caused by poor posture.
5. Relaxation techniques:
- Progressive muscle relaxation and guided visualization.
Benefits:
- It reduces anxiety and panic during an asthma attack.
- It promotes efficient breathing patterns.
6. Education and self-management:
Techniques:
- Teaching proper inhaler techniques.
- Providing training on recognizing early signs of an asthma attack.
Benefits:
- It empowers patients to manage their condition independently.
- It reduces reliance on emergency medical interventions.
7. Pulmonary Rehabilitation.
- Components: Comprehensive program combining breathing exercises, physical training, and education.
Benefits:
- It improves lung function and exercise tolerance.
- It enhances the overall quality of life in moderate to severe asthma cases.
8. Biofeedback:
- Techniques: Uses devices to monitor breathing patterns and provides feedback for correction.
Benefits:
- It helps patients gain control of dysfunctional breathing patterns.
- It prevents hyperventilation-related symptoms.
Overall benefits of Physiotherapy in Asthma:
- Improved breathing control.
- Better Airway clearance.
- Reduced symptoms.
- Increased exercise tolerance.
- Anxiety and stress reduction.
- Enhanced posture.
- Improved quality of life.
ROLE OF ACUPUNCTURE IN ASTHMA:
Acupuncture is an ancient Chinese medical technique that involves inserting sterile needles into specific points on the body, known as acupoints. It is based on restoring balance and energy flow(Qi or Chi)through meridians, or pathways, in the body. When used for asthma, acupuncture aims to improve lung function, reduce inflammation, and modulate the immune response.
Techniques in Acupuncture for Asthma:
1. Needling specific Acupoints:
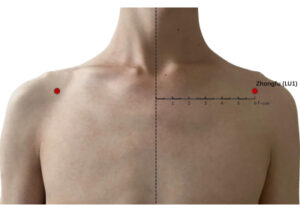
- LU1(Zhongfu): Improves lung function and relieves respiratory symptoms.
- LU7(Lieque): Clears lung meridian and helps to expel mucus.
- CV17(Shanzhong): Relieves chest tightness and promotes better breathing.
- BL13(Feishu): Enhances the respiratory system and supports lung energy.
- ST36(Zusanli): Strengthens overall energy and immunity.
2. Electroacupuncture:
- This technique involves attaching small electrodes to acupuncture needles to deliver a mild electric current, enhancing the stimulation of acupoints and providing greater therapeutic effects.
Benefits of Acupuncture in Asthma:
- It improves lung function.
- Reduces inflammation.
- Decreases bronchial hyperresponsiveness.
- Relieves stress and anxiety.
- Balances the immune system.
- Improves sleep quality.
- Reduces medication dependence.
- Enhances quality of life.
ROLE OF YOGA AND PRANAYAMA IN ASTHMA:
Yoga and Pranayama play a significant role in managing asthma by improving lung function, reducing stress, and enhancing overall respiratory efficiency. It can also complement conventional treatments by addressing both physical and psychological aspects of asthma.
TECHNIQUES AND BENEFITS OF YOGA:
Yoga combines physical postures, breathing exercises, and meditation to promote holistic well-being. In asthma, it helps by improving lung capacity, reducing stress, and enhancing airway function.
I)Asanas(Postures) for Asthma:
Certain yoga postures specifically target the respiratory system.
a) Bhujangasana(Cobra pose):
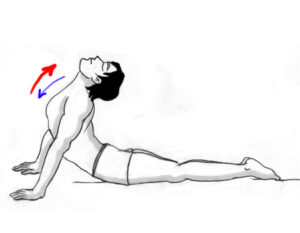
- It expands the chest and improves lung function. It strengthens the diaphragm and relieves chest tightness.
b) Matsyasana(Fish pose):

- It opens up the chest and throat area, enhancing airflow and easing breathing.
c) Setu bandh asana(Bridge pose):
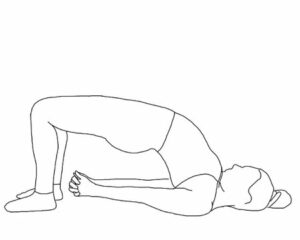
- Improves chest expansion, lung ventilation, and oxygen delivery.
d) Ardha Matsyendrasa(Half spinal twist):

- Promotes better lung function by twisting the torso and aiding respiratory mechanics.
e) Dhanurasana(Bow pose):

- Strengthens the lungs and reduces bronchial congestion.
f) Tadasana(Mountain pose):
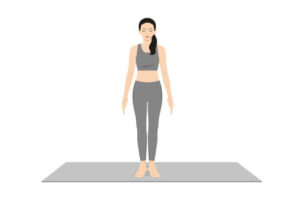
- It enhances posture, opens the chest, and improves lung efficiency.
Benefits of Yoga for Asthma:
- Improved lung function. Yoga increases chest flexibility, allowing better expansion of the lungs.
- Stress reduction: Stress is a known asthma trigger. Yoga calms the mind and reduces anxiety.
- Improved oxygen utilization: Enhances the efficiency of oxygen exchange in the lungs.
- Postural alignment: Poor posture can restrict breathing. Yoga improves alignment, aiding lung expansion.
- Strengthened respiratory muscles: Builds strength in muscles like the diaphragm, which is essential for breathing.
TECHNIQUES AND BENEFITS OF PRANAYAMA IN YOGA:
Pranayama involves controlled breathing techniques that improve lung capacity, regulate breathing patterns, and calm the nervous system. It is especially effective for asthma patients as it trains them to control their breath during an attack.
Techniques:
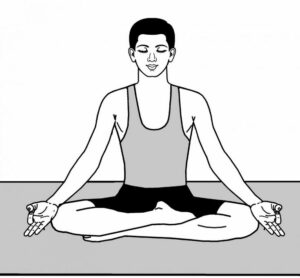
1. Nadi Shodhana(Alternate nostril breathing):
- Balances airflow between nostrils.
- Clears nasal passages and promotes efficient breathing.
2. Anuloma Viloma(Alternate nostril breathing without retention):
- It helps reduce airway constriction and improves oxygenation.
3. Bhastrika(Bellows breathing):
- Strengthens respiratory muscles and clears mucus from the airways.
4. Kapalbhati(Skull shining breathing):
- Expels stale air from the lungs, improves lung elasticity, and detoxifies the respiratory system.
5. Brahmari(bee breathing):
- It creates a calming effect on the mind and reduces stress-induced asthma symptoms.
6. Ujjayi(ocean sound breathing):
- Controls airflow and slows down breathing, which is particularly helpful during wheezing episodes.
7. Deep diaphragmatic breathing:
- Encourages full oxygen exchange and strengthens the diaphragm.
Benefits of Pranayama for Asthma:
- Improves breathing efficiency.
- Reduces airway resistance.
- Detoxifies the lungs.
- Enhances the lung capacity.
- Calms the nervous system.
- Reduces hypersensitivity.
Precaution for Asthma patients:
- Whenever possible, especially in the beginning, practice yoga and pranayama under the supervision of a qualified instructor.
- Holding your breath for too long during pranayama can make your symptoms worse.
- Avoid being exposed to asthma triggers, practice in a clean, dust-free area.
- Begin with mild methods and gradually indulge in strenuous methods as your lung capacity increases.
DIETARY REGIMEN IN ASTHMA:
- Avoid cold, heavy, and mucus-forming foods.
- Eat warm, freshly cooked meals.
- Avoid leftover, frozen, or canned foods.
- Drink warm water, that helps in clearing mucus and improving digestion.
- Consume meals at regular intervals because the gap between meals might aggravate acidity which can worsen asthma.
DISCLAIMER: The information provided in this article is intended solely for educational purposes. Treatment decisions should be made exclusively by a well-qualified Ayurvedic physician. Self-medication is strongly discouraged.
Maurya Ayurveda Hospital,opposite to Sabine Hospital,Pezhakkapilly P.O,Muvattupuzha,Ernakulam;PIN:686673,Contact no:9947183000
Email: info@mauryaayurveda.com
Maurya Ayurveda Ortho & Neuro Rehabilitation Centre ( Ayurveda Hospital )